
2026 Open Enrollment ended on November 14, 2025. Review the information under Open Enrollment Aftercare for next steps.
Once Open Enrollment ends, there are several important things that will be happening that you should know about.
A digital copy of your 2026 Open Enrollment Confirmation Statement will be posted in myACI in Document Records. A printed copy of your 2026 Open Enrollment Confirmation Statement will not be mailed to your home. Associates who do not have a work email address on file or have not opted in to receive email notifications via their personal email address will receive a postcard at their home with instructions on how to access the Confirmation Statement in myACI in Document Records.
Your Confirmation Statement will include your 2026 benefits enrollment and paycheck deductions, information on your covered dependents and your beneficiary designations. If any information on your Confirmation Statement is incorrect, you will have until December 12, 2025 to report it to the Associate Experience Center. You can speak to a Representative Monday-Friday, 6 a.m to 6 p.m. AZ time by calling 888-255-2269.
Your coverage will take effect on January 1, 2026.
To view your confirmation statement, go to myACI.albertsons.com. From the Me page, click on the Benefits tile then click on Document Records in the Quick Actions sidebar. To find your statement, look for the most recent document labeled as Document type “Benefits Letter.”
To review your benefits and coverage information in myACI as of January 1, visit myACI.albertsons.com. From the Me page, click on the Benefits tile. Under “Show Benefits”, select “As of date” and select 01/01/2026.
To see if you have any Pending Actions, sign in to your account at myACI.albertsons.com. Choose the Benefits tile. If you have any pending actions, they will be displayed above your Enrollment Summary.
Access the Pending Actions Quick Reference Guide (QRG) for step-by-step assistance in completing pending actions in myACI.
Pending Action for Newly Enrolled Dependents: If you enrolled any dependents for the first time during Open Enrollment, you must provide documentation verifying their eligibility. You can download a Dependent Verification Requirements Flyer which lists the allowable documents you can submit to verify your dependent’s eligibility to be covered under Albertsons healthcare plans. Dependent verification must be completed by January 31, 2026. If you miss the deadline, your unverified dependents will not be covered in 2026 unless you experience a qualifying life event during the year.
To see if you have any Pending Actions, sign in to your account at myACI-albertsons.com. Choose the Benefits tile. If you have any pending actions, they will be displayed above your Enrollment Summary.
EOI for Optional Life Insurance or Long-term Disability Coverage
If you have enrolled in optional life insurance for yourself or your spouse or domestic partner or long-term disability for yourself that requires evidence of insurability (EOI), please note the following:
- Email communication from The Hartford will be sent by December 8 (or printed communication mailed to your home if no email address is on file). The communication will provide instructions on what you need to do to provide evidence of insurability (EOI) within the 60-day enrollment window.
- Complete an online Personal Health Application (PHA) within 60 days from the date you are notified by The Hartford via email or printed communication mailed to your home to complete an online PHA. If The Hartford approves your coverage request, coverage and paycheck deductions will start as soon as administratively possible within 1 or 2 pay periods following the approval date. If The Hartford does not approve your coverage request, you will be notified by The Hartford, and your request for coverage (or increase in coverage) will be canceled.
How to Complete EOI Online
- Visit: https://www.myhartfordbenefits.com/onlineeoi/albertsons and follow the initial login instructions.
- Username: First letter of your first name + first letter of your last name + last 4 digits of your SSN Example: John Smith, SSN XXX-XX-4321 → js4321
- Password: First letter of your first name + first letter of your last name + date of birth (YYYYMMDD) Example: John Smith, DOB October 25, 1963 → js19631025
Multifactor Authentication (MFA)
To enhance the security of your account and protect sensitive information, The Hartford requires a second authentication method in addition to your username and password. The Hartford will send you an authentication code which you can receive:
- By text message sent your mobile phone;
- By email; or
- By a phone call to your mobile phone
If you do not have a mobile phone number or email address registered with The Hartford, call 877-663-4278 to verify your identity and receive an authentication code over the phone.
Note: If enrolling a Spouse or Domestic Partner, use their demographic information to create their login credentials. If you spouse or domestic partner needs to complete EOI, they will also require MFA. The Hartford will send an authentication code to an associate’s email address (if available). Otherwise, your spouse or domestic partner can call The Hartford at 877-663-4278 to receive an authentication code over the phone.
If you enrolled in the HSA or Kaiser CA HSA Plan for the first time during Open Enrollment and you want to set up contributions, you must open a health savings account (HSA) with Fidelity to make pre-tax contributions via paycheck deduction that you can use to pay for eligible health care expenses.
Action Steps
- Watch for communication from Fidelity.
– You will receive an email (or printed communication mailed to your home if no email address is on file) from Fidelity by November 28. The communication will include instructions on how to open your HSA. - Open your Fidelity HSA.
– Visit netbenefits.com and log in, or follow the instructions to register as a new user.
– Click the “Open” tile to begin the account setup process.
Important Note: If your HSA enrollment information is not yet available in Fidelity, you will not see a link on netbenefits.com to open an account. Visit Fidelity.com to establish a personal HSA. Once your enrollment information and data are loaded in Fidelity, your personal HSA will be automatically linked to your ACI-sponsored HSA. No additional action is required on your part. - Verify your HSA contributions.
– Once deductions begin, confirm that the HSA contribution amount is correct on your paycheck and that funds are available in your Fidelity HSA.
If you open your HSA after December 26, paycheck deductions will start as soon as administratively possible (usually 1 or 2 pay periods after your HSA is opened).
You can start, stop or change your HSA contributions at any time by signing in to myACI.albertsons.com. Click on the Benefits tile, then click on Report a Life Event or HSA Change under the Quick Actions sidebar.
To speak to a Fidelity HSA Specialist, call 866-956-3433 Monday-Friday, 6 am to 8 pm MT or Saturday-Sunday, 7 am to 2 pm MT.
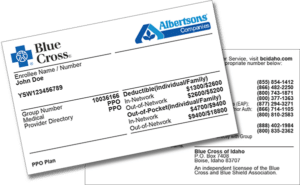
- If you are enrolled in a BCI medical plan, you will receive new ID cards for 2026 if your plan has a change in the annual deductible or out-of -pocket maximum.
- If you newly enrolled in an Albertsons Companies medical plan or you changed medical plans during Open Enrollment, you will receive new ID cards from your medical plan provider.
- BCI mailed new 2026 ID cards on Tuesday, December 16.
- If you enrolled in a Blue Cross of Idaho (BCI) medical plan, SelectHealth HMO or HMSA for the first time during Open Enrollment or you changed your BCI medical plan, you will receive a separate pharmacy ID card from MedImpact, our pharmacy benefits manager.
- If you did not change medical plans during Open Enrollment and the plan you are enrolled in does not have a change in deductible or out-of-pocket maximum for 2026, you can continue using your current medical ID card.
Most of our insurance carriers and vendor partners have mobile apps available making it easy and convenient for you to schedule appointments, access digital ID cards, check on the status of claims, confirm account balances and much more. Links to insurance carrier apps from the App Store and Google Play are available at https://myaci-benefits.com/resources/mobileapps/.

